Why Pregnancy Care Feels Overwhelming — And How I Learned to Trust Myself
Pregnancy should be joyful, but for me, it came with endless worries — am I eating right? Moving enough? Staying emotionally balanced? I quickly realized that real pregnancy care isn’t about perfection — it’s about awareness. This journey taught me to listen to my body, make informed choices, and build daily habits that support both my health and my baby’s. Here’s what actually helped.
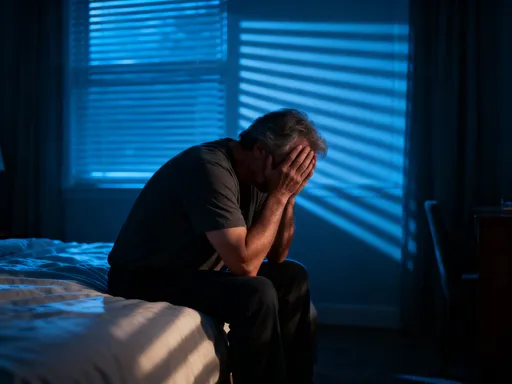
The Hidden Stress of “Perfect” Pregnancy Expectations
From the moment a pregnancy test turns positive, the world seems to offer endless rules. Eat this, avoid that. Rest more, but stay active. Stay calm, even when everything feels uncertain. These messages, often repeated by well-meaning friends, online communities, or even healthcare providers, can create an invisible standard of the "perfect pregnancy." The pressure to meet this ideal is real, and for many women, it becomes a source of quiet distress rather than empowerment. The truth is, no two pregnancies are the same, and expecting uniformity only increases anxiety and self-doubt.
Modern culture often amplifies this pressure through curated social media feeds, where glowing mothers-to-be share smoothie recipes, prenatal workout routines, and serene meditation practices. While these can be inspiring, they rarely show the full picture — the fatigue, the nausea, the moments of fear or doubt. This selective portrayal can distort expectations, making ordinary struggles feel like personal failures. When a woman feels too tired to cook a "perfect" organic meal or skips a yoga session because she’s overwhelmed, she may interpret these small choices as falling short, when in reality, they are part of a normal, healthy experience.
What many don’t realize is that the pursuit of perfection can actually undermine well-being. Constant self-monitoring and fear of making a "wrong" choice can elevate stress hormones like cortisol, which, when chronically high, may affect both maternal and fetal health. Research in perinatal psychology suggests that excessive worry about diet, weight, or behavior during pregnancy is linked to increased anxiety and lower satisfaction with the pregnancy experience. The goal, then, is not to eliminate care or caution, but to shift the focus from rigid compliance to compassionate awareness.
Self-compassion is not a luxury — it’s a foundational element of healthy pregnancy care. It means recognizing that fatigue is not laziness, that occasional cravings are not moral failings, and that emotional fluctuations are not signs of weakness. By treating oneself with the same kindness one would offer a close friend, a woman can begin to release the burden of unrealistic expectations. This mental shift doesn’t mean ignoring health guidelines; rather, it means engaging with them from a place of self-respect rather than fear. Letting go of perfection is not surrender — it’s the first step toward sustainable, personalized care.
Listening to Your Body: The Most Important Skill No One Talks About
In a world filled with pregnancy apps, tracking tools, and expert advice, one of the most powerful resources is often overlooked: the body’s own signals. While charts and guidelines offer useful frameworks, they cannot replace the nuanced, real-time feedback that a woman receives from her own physical and emotional experience. Learning to interpret these signals — fatigue, hunger, mood changes, physical discomfort — is a skill that builds confidence and supports informed decision-making throughout pregnancy.
Consider fatigue, one of the most common yet misunderstood symptoms. Many women feel guilty for needing more rest, especially in the first trimester when outward changes are minimal. But fatigue is not a flaw — it is a biological signal that the body is working hard to support a growing life. Ignoring it can lead to burnout, while honoring it can prevent unnecessary strain. Similarly, food cravings or aversions are often dismissed as whims, but they can reflect genuine nutritional needs or the body’s way of protecting itself from certain foods during sensitive developmental stages. A sudden dislike for coffee or strong smells, for instance, may be linked to heightened sensitivity that helps avoid potential irritants.
Emotional shifts are equally important. Mood swings, irritability, or moments of sadness are not signs of instability — they are natural responses to hormonal fluctuations and the psychological weight of impending motherhood. When these feelings are pathologized or suppressed, they can grow into deeper distress. But when acknowledged with curiosity rather than judgment, they become valuable data points. A woman who notices that she feels calmer after a short walk or more anxious after scrolling through social media is gathering insight that no app can provide.
Body literacy — the ability to understand and respond to these internal cues — is a form of empowerment. It transforms pregnancy from a passive experience of following rules into an active process of self-awareness. This doesn’t mean rejecting medical advice; rather, it means integrating it with personal experience. For example, if a prenatal vitamin causes nausea, instead of enduring discomfort, a woman might try taking it at night or switching formulations — a small adjustment made possible by listening. Over time, this practice builds trust in one’s own instincts, laying the foundation for confident parenting beyond pregnancy.
Daily Habits That Actually Support Pregnancy Wellness
Amid the noise of extreme diets and intense workout trends, the most effective pregnancy care often lies in simple, consistent habits. Lasting wellness is rarely the result of dramatic changes but of small, sustainable choices repeated over time. These daily routines, when grounded in science and adapted to individual needs, create a stable foundation for both mother and baby.
Nutrition is central, but it doesn’t require perfection. A balanced approach emphasizing whole foods — fruits, vegetables, whole grains, lean proteins, and healthy fats — provides the essential nutrients for fetal development and maternal energy. Folic acid, iron, calcium, and omega-3 fatty acids are particularly important, and while supplements can help fill gaps, food should remain the primary source. Instead of focusing on restriction, the goal is nourishment. Eating regular, balanced meals helps stabilize blood sugar, reducing fatigue and mood swings. Snacks like nuts, yogurt, or fruit can prevent excessive hunger, which often leads to overeating or poor choices later.
Hydration is another cornerstone. Water supports amniotic fluid production, nutrient transport, and digestion. Dehydration can contribute to headaches, constipation, and even preterm contractions in extreme cases. While the "eight glasses a day" rule is a helpful guideline, individual needs vary. A simple indicator is urine color — pale yellow suggests adequate hydration, while darker shades signal the need for more fluids. Herbal teas, broths, and water-rich foods like cucumbers and oranges also contribute to fluid intake.
Sleep and rest are equally vital. Quality sleep supports immune function, hormone regulation, and emotional resilience. As pregnancy progresses, physical discomfort can make rest challenging, but good sleep hygiene can help. Establishing a consistent bedtime, limiting screen time before bed, and using supportive pillows can improve comfort. Short naps, when possible, can compensate for nighttime disruptions. Movement, too, plays a role — gentle physical activity during the day often leads to better sleep at night.
These habits are not about achieving an ideal routine but about creating a rhythm that fits real life. A working mother may not have time to cook elaborate meals, but she can prepare simple, nutritious options in advance. A woman with young children may not get eight hours of uninterrupted sleep, but she can prioritize rest when opportunities arise. The key is consistency, not perfection. Over time, these small actions accumulate, forming a resilient foundation for pregnancy and beyond.
Movement Without Fear: Finding Joy in Physical Activity
For many pregnant women, the idea of exercise comes with hesitation. Stories of restrictions, warnings about overheating, or fears of harming the baby can make physical activity feel risky. Yet, when approached with awareness, movement is one of the most beneficial aspects of pregnancy care. The American College of Obstetricians and Gynecologists recommends at least 150 minutes of moderate-intensity aerobic activity per week for most pregnant women, citing benefits for cardiovascular health, mood, and energy levels.
Gentle, regular movement supports circulation, reducing the risk of swelling and varicose veins. It strengthens muscles needed for labor and recovery, improves posture, and can even help regulate blood sugar, lowering the risk of gestational diabetes. Perhaps most importantly, physical activity is a powerful tool for emotional well-being. Exercise releases endorphins, natural chemicals that reduce stress and enhance mood. For women dealing with anxiety or low energy, even a short walk can bring noticeable relief.
The key is choosing activities that feel safe and enjoyable. Walking is one of the most accessible and effective options — it requires no special equipment, can be done at any stage of pregnancy, and easily fits into daily life. Prenatal yoga and swimming are also excellent choices, offering low-impact movement that supports flexibility and relaxation. Strength training, when done with proper form and guidance, helps maintain muscle tone and joint stability. The goal is not intensity but consistency and comfort.
Common concerns — such as overheating, joint pain, or balance issues — can be managed with simple adjustments. Staying hydrated, wearing breathable clothing, and avoiding exercise in extreme heat reduce the risk of overheating. As the body’s center of gravity shifts, movements that challenge balance should be modified or avoided. Listening to the body is essential — if an activity causes pain, dizziness, or shortness of breath, it’s a signal to slow down or stop. Women with certain medical conditions should consult their healthcare provider before beginning or continuing an exercise routine, but for most, staying active is not only safe but recommended.
Shifting the mindset from "exercise as obligation" to "movement as self-care" can transform the experience. A walk in nature, a stretch session with calming music, or a gentle dance in the kitchen with a child — these moments are not just physical activity; they are acts of presence and connection. When movement feels joyful rather than forced, it becomes a natural part of daily life, supporting both physical health and emotional balance.
Emotional Health as Core Pregnancy Care
Emotional well-being is not a secondary concern during pregnancy — it is central to the health of both mother and baby. Stress, anxiety, and isolation are common, yet often minimized or dismissed as "just hormones." But the mind and body are deeply connected. Chronic stress can influence hormone levels, sleep patterns, and even immune function, potentially affecting fetal development. Recognizing emotional health as an essential part of prenatal care allows women to address these challenges proactively and with compassion.
Anxiety about the baby’s health, labor, parenting, or life changes is normal, especially for first-time mothers. But when worry becomes overwhelming, it can interfere with daily functioning and enjoyment of pregnancy. Feelings of sadness, irritability, or emotional numbness may also arise, and while they don’t always indicate clinical depression, they should not be ignored. The perinatal period is a time of heightened vulnerability, and early attention to emotional symptoms can prevent more serious concerns later.
Non-clinical strategies can make a meaningful difference. Journaling, for example, provides a safe space to process thoughts and emotions. Writing down worries, hopes, or daily reflections helps externalize internal struggles, making them easier to understand and manage. Mindful breathing exercises — such as slow, deep breaths for a few minutes each day — can activate the parasympathetic nervous system, promoting relaxation and reducing anxiety. Even simple practices like pausing to notice the breath, the sounds around, or the sensation of feet on the ground can bring a sense of calm.
Social connection is another powerful support. Talking with trusted friends, joining a prenatal group, or sharing feelings with a partner can reduce isolation and provide reassurance. Many women hesitate to express doubts or fears, worried they’ll be judged or seen as ungrateful. But opening up often reveals that others feel the same way, creating space for mutual support. When emotional challenges persist or intensify, seeking help from a therapist or counselor is a sign of strength, not weakness. Mental health care during pregnancy is not just acceptable — it is a vital part of comprehensive care.
Navigating Information Overload: What to Trust, What to Skip
In the age of instant information, pregnancy advice is everywhere — from online forums and parenting blogs to family traditions and celebrity endorsements. While access to knowledge is valuable, the sheer volume of conflicting recommendations can be overwhelming. One source says coffee is safe in moderation; another claims it must be avoided entirely. One blog promotes a strict elimination diet; another emphasizes balance and flexibility. Sorting through this noise requires critical thinking and a clear sense of what constitutes reliable guidance.
The first step is evaluating sources. Medical guidelines from reputable organizations — such as the American College of Obstetricians and Gynecologists, the World Health Organization, or national health services — are based on rigorous research and expert consensus. These should form the foundation of decision-making. In contrast, anecdotal advice, viral trends, or products marketed with dramatic claims often lack scientific support. Red flags include promises of "miracle" results, fear-based messaging, or recommendations that contradict established medical guidance.
When encountering new information, it’s helpful to ask a few key questions: Who is sharing this? What evidence supports it? Does it align with my healthcare provider’s advice? Is it personalized to my situation, or is it a one-size-fits-all claim? For example, a study cited in a blog post may sound convincing, but if it’s based on a small sample or not replicated, its relevance may be limited. Similarly, a supplement promoted as "natural" is not necessarily safe — some herbs and compounds can interact with pregnancy in harmful ways.
The role of the healthcare provider is crucial in this process. Regular prenatal visits offer a consistent, personalized source of guidance. Women should feel empowered to discuss concerns, ask questions, and seek clarification on conflicting advice. A good provider listens, respects autonomy, and supports informed decision-making. They can help interpret test results, explain risks and benefits, and offer recommendations tailored to individual health history.
Ultimately, the goal is not to eliminate all uncertainty — some aspects of pregnancy will always involve unknowns — but to build confidence in one’s ability to navigate them. Curiosity is valuable, but it should be balanced with discernment. By focusing on evidence-based awareness rather than viral trends, women can make choices that are informed, intentional, and aligned with their values.
Building a Personalized Pregnancy Plan That Grows With You
Every pregnancy is unique, shaped by individual health, lifestyle, and personal circumstances. A rigid, one-size-fits-all plan may work for some, but for most women, flexibility is key. The most effective approach is not a fixed schedule but an adaptable framework that evolves with changing needs across trimesters. This personalized plan integrates medical guidance, daily habits, emotional awareness, and practical adjustments to support long-term well-being.
The first step is self-reflection. What are your energy levels like? What activities bring you joy or relief? What stressors are present in your daily life? Tracking these factors — through a journal, app, or simple notes — helps identify patterns and informs better choices. For example, if fatigue peaks in the afternoon, scheduling rest during that time may be more effective than pushing through. If certain foods consistently cause discomfort, adjusting the diet becomes a logical response rather than a source of guilt.
Professional input remains essential. Regular check-ups provide objective data — weight gain, blood pressure, fetal growth — that complements personal observations. Discussing symptoms, concerns, and goals with a healthcare provider ensures that the plan stays medically sound. This collaboration creates a safety net, allowing for both autonomy and expert oversight.
As pregnancy progresses, needs change. The first trimester may focus on managing nausea and fatigue, while the second allows for increased activity and social engagement. The third often requires adjustments for comfort, rest, and preparation for labor. A flexible plan acknowledges these shifts, allowing for modifications without self-judgment. It may include different movement routines, evolving nutrition goals, or changing emotional support strategies.
Perhaps most importantly, this approach fosters health consciousness that extends beyond delivery. The habits, awareness, and self-trust developed during pregnancy can support postpartum recovery, parenting, and long-term well-being. By focusing on presence rather than perfection, women build a foundation not just for a healthy pregnancy, but for a resilient, empowered life.
Pregnancy care isn’t about following a strict script — it’s about developing awareness, making intentional choices, and trusting your inner voice. By focusing on practical, sustainable habits and emotional resilience, women can move from anxiety to empowerment. True health consciousness isn’t perfection — it’s presence.