The Quiet Wake-Up Call: What I Learned Before My Body Shut Down
I used to think "feeling tired" was just part of adult life—until my doctor said I was on the edge of something serious. That moment changed everything. What I thought were normal habits were actually silent red flags. This is the real talk about lifestyle pitfalls and how catching them early saved me from a full-blown health crisis. No scare tactics—just honest lessons learned the hard way. It wasn’t a heart attack or diagnosis that stopped me in my tracks, but a simple blood test that revealed inflammation, elevated glucose, and warning signs no one could ignore. The truth? My body had been sending messages for years. I just wasn’t listening. This is what happens when daily choices quietly erode health—and how awareness, not fear, can bring it back.
The Normal That Wasn’t
For years, life ran on autopilot. Mornings began with coffee on the go, lunch was skipped or eaten at the desk, and evenings blurred into screen time and takeout. Fatigue wasn’t a signal—it was a given. Many women in their thirties, forties, and fifties live this way, juggling family, work, and responsibilities with little thought to how these patterns affect long-term health. The problem isn’t any single choice, but the slow accumulation of behaviors that feel normal yet slowly deplete the body’s reserves. Poor sleep, chronic stress, and irregular eating aren’t quirks of modern life—they’re foundational risks.
What makes these habits so dangerous is their invisibility. When everyone around you is running on empty, exhaustion becomes a badge of honor. "I’m so busy" turns into a default explanation for irritability, low energy, and brain fog. But the body doesn’t adapt to constant strain—it adapts until it can’t. Over time, cortisol levels remain elevated, digestion weakens, and immune function dips. These aren’t dramatic failures; they’re gradual declines masked as normalcy. The real danger lies in mistaking endurance for health. Just because you can keep going doesn’t mean you should.
Many women reach midlife having spent years prioritizing others—children, partners, parents, employers—while quietly neglecting their own well-being. The cost isn’t always immediate, but it compounds. Missing meals leads to blood sugar swings. Poor sleep impairs cellular repair. Emotional stress without release fuels systemic inflammation. These aren’t isolated issues—they’re interconnected threads in a larger pattern of imbalance. Recognizing that "normal" doesn’t mean "healthy" is the first step toward change. It’s not about guilt or blame, but awareness. The body is resilient, but it’s not indestructible.
When “Fine” Isn’t Fine: Recognizing Early Signals
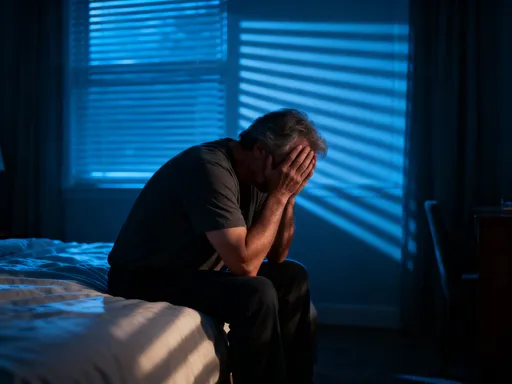
Most serious health conditions don’t arrive suddenly. They develop silently, often for years, before symptoms become undeniable. The body sends early warnings—fatigue that doesn’t lift with rest, joint stiffness that lingers, mood shifts that feel out of sync with life circumstances. These aren’t just signs of aging or stress. They’re biological messages indicating that something is off balance. Persistent tiredness, for example, isn’t just about sleep. It can signal hormonal imbalances, nutrient deficiencies, or early metabolic dysfunction. The challenge is that these signals are easy to dismiss, especially when life feels demanding.
Science shows that long before disease is diagnosed, the body undergoes preclinical changes—alterations in blood markers, inflammation levels, and organ function that don’t yet meet diagnostic thresholds. These are the quiet phases where intervention can make the biggest difference. Elevated fasting glucose, for instance, may not mean diabetes yet, but it’s a clear indicator of insulin resistance. Slightly high blood pressure isn’t a diagnosis, but it’s a sign the cardiovascular system is under strain. These are not emergencies, but they are invitations to act.
Listening to these signals requires a shift in mindset. Instead of waiting for a crisis, it means tuning in to subtle shifts in energy, digestion, sleep quality, and emotional well-being. A woman who used to handle stress with ease but now feels overwhelmed by small challenges may be experiencing adrenal fatigue. Someone who never had digestive issues but now feels bloated after meals might be developing food sensitivities or gut imbalance. These aren’t minor inconveniences—they’re clues. The body communicates through sensation, and learning to interpret those signals is a form of self-respect.
One of the most powerful tools is tracking. Not obsessively, but mindfully. Keeping a simple journal of energy levels, mood, sleep, and food intake can reveal patterns invisible in the moment. A week of low energy following poor sleep or high sugar intake isn’t coincidence—it’s cause and effect. Recognizing these patterns builds self-awareness, which is the foundation of prevention. You don’t need to be a doctor to notice when something feels off. You just need to pay attention.
The Myth of the Quick Fix
In a world that values speed and convenience, it’s no surprise that many turn to quick fixes when health starts to falter. Detox teas, miracle supplements, juice cleanses, and crash diets promise fast results with minimal effort. The appeal is understandable—when you’re exhausted and overwhelmed, the idea of a simple solution is comforting. But these approaches rarely address the root causes of declining health. They may offer temporary relief or short-term weight loss, but they don’t create lasting change. Worse, they can reinforce the belief that health is something to be fixed, not maintained.
Real health transformation isn’t about extreme measures. It’s about consistency, not intensity. The body thrives on routine, balance, and sustainability. A three-day juice cleanse won’t undo years of poor nutrition, just as a month of intense workouts won’t compensate for chronic stress and sleep deprivation. The danger of quick fixes isn’t just their ineffectiveness—they can also delay meaningful action. Chasing the next trend keeps you focused on symptoms rather than causes, and the underlying habits that led to imbalance remain unchanged.
Supplements, for example, can play a supportive role when used appropriately, but they are not substitutes for a healthy lifestyle. Taking a vitamin D pill won’t compensate for lack of sunlight, poor diet, or indoor living. Omega-3s can help reduce inflammation, but they can’t counteract a diet high in processed foods and sugar. These tools work best when integrated into a broader strategy, not as standalone solutions. The same goes for detoxes. The liver and kidneys are already designed to filter toxins—the best way to support them is through hydration, whole foods, and reduced exposure to processed chemicals, not short-term cleanses.
The real work happens in the daily choices: what you eat, how you move, how you rest, and how you manage stress. These aren’t glamorous or viral, but they are powerful. Lasting change comes from small, repeatable actions that become habits over time. It’s not about perfection. It’s about progress. And progress doesn’t come from quick fixes—it comes from commitment to the process.
Rewriting My Routine: What Actually Worked
After my wake-up call, I didn’t overhaul everything at once. That would have been overwhelming and unsustainable. Instead, I focused on small, manageable changes that could become part of my daily rhythm. The first shift was in how I measured success. I stopped fixating on the scale and started paying attention to energy levels. How did I feel by mid-afternoon? Was I reaching for coffee or snacks to stay alert? Did I wake up rested? These became my real metrics of health.
Mindful eating was a game-changer. I began eating regular meals, sitting down without distractions, and chewing slowly. I prioritized whole foods—vegetables, fruits, lean proteins, healthy fats—and reduced processed items. I didn’t eliminate anything completely, but I became more intentional. Instead of skipping breakfast, I prepared simple options like oatmeal with nuts or eggs with avocado. Lunch moved away from the desk and into a quiet space. These weren’t drastic changes, but they added up. Digestion improved, energy stabilized, and cravings decreased.
Movement became part of my day in small doses. I stopped thinking of exercise as something that required a gym or 45-minute class. Instead, I built in "movement snacks"—short walks after meals, stretching in the morning, taking the stairs. Ten minutes of walking after dinner helped with digestion and cleared my mind. Over time, these moments added up to consistent activity without feeling like a chore. The goal wasn’t to burn calories, but to keep the body active and circulation flowing.
Sleep hygiene was another key shift. I set a consistent bedtime and created a wind-down routine—dimming lights, turning off screens an hour before bed, and reading or journaling instead. I invested in blackout curtains and kept the bedroom cool. These small environmental tweaks made a noticeable difference in sleep quality. I also learned to say no to late-night obligations that disrupted rest. Protecting sleep became non-negotiable, not a luxury.
Habit stacking helped make these changes stick. I paired new behaviors with existing ones—drinking a glass of water after brushing my teeth, doing five minutes of stretching after turning off the coffee maker. I also redesigned my environment to support better choices—keeping fruit on the counter, placing walking shoes by the door, and removing processed snacks from the pantry. These weren’t willpower wins—they were design wins. The easier I made the healthy choice, the more likely I was to follow through.
The Role of Check-Ins—Before the Breakdown
One of the most important lessons I learned was the value of proactive health check-ins. I used to wait for symptoms before seeing a doctor. Now, I go regularly, even when I feel fine. Annual physicals, blood work, and preventive screenings are not signs of illness—they’re tools of awareness. They provide objective data about what’s happening inside the body, often revealing issues long before symptoms appear.
Blood tests, for example, can detect early signs of inflammation, insulin resistance, thyroid imbalances, and nutrient deficiencies. A simple lipid panel can show trends in cholesterol that, if addressed early, can prevent cardiovascular issues down the line. These tests aren’t about fear—they’re about information. Knowledge is power, and having a baseline makes it easier to track changes over time. It also allows for earlier, less invasive interventions—lifestyle adjustments instead of medications.
Honest conversations with healthcare providers are just as important. I learned to prepare for appointments with questions and observations—tracking my energy, sleep, and any new symptoms. I stopped downplaying concerns because they “didn’t seem serious.” Small changes matter. A doctor can connect dots that might not be obvious on your own. For example, persistent fatigue combined with dry skin and weight gain could point to thyroid issues. Joint pain and bloating might signal food sensitivities or gut inflammation. These connections are easier to spot with professional guidance.
Prevention isn’t about avoiding illness at all costs—it’s about building resilience. Regular check-ins are part of that. They reinforce the idea that health is an ongoing process, not a destination. They also reduce the anxiety of the unknown. When you have data, you’re not guessing. You’re making informed decisions. And that makes it easier to take action before small issues become big problems.
Environment Over Willpower
One of the biggest misconceptions about health is that it’s all about discipline. The truth is, willpower is limited. Lasting change depends more on environment than motivation. If your kitchen is stocked with processed foods, your workspace demands long hours, and your evenings are filled with screen time, no amount of willpower will make healthy choices easy. But when the environment supports better habits, those choices become automatic.
I began by making small changes at home and work. I cleared my pantry of sugary snacks and replaced them with nuts, seeds, and whole-grain options. I kept a water bottle on my desk to stay hydrated. I set reminders to stand and stretch every hour. At home, I created a charging station outside the bedroom to reduce screen time before bed. These weren’t heroic efforts—they were practical adjustments that made the healthy choice the default choice.
Workplace culture can be a challenge, especially in desk-based jobs. Long hours, sedentary routines, and constant demands contribute to physical and mental strain. I started advocating for small breaks—walking meetings when possible, standing during phone calls, and stepping outside for fresh air. I also learned to set boundaries around work hours to protect personal time. These changes didn’t require approval—they just required intention.
Social environments matter too. I became more mindful of how gatherings revolved around food and drink. Instead of avoiding them, I planned ahead—eating a healthy meal beforehand, bringing a nutritious dish to share, or suggesting non-food-centered activities like walks or coffee dates. This way, I could enjoy connection without compromising my goals. The goal wasn’t restriction, but balance.
Designing a supportive environment isn’t about perfection. It’s about making small, consistent improvements that reduce friction. When healthy choices are easy, they become habitual. And habits, not willpower, are what sustain long-term health.
A Lifestyle That Lasts: Building Resilience, Not Perfection
The final shift in my journey was a change in mindset. I stopped viewing health as a problem to be solved and started seeing it as a foundation to be nurtured. This isn’t about achieving a perfect body or eliminating all stress. It’s about building resilience—the ability to adapt, recover, and thrive despite life’s challenges. Resilience comes from consistency, not intensity. It’s built through daily acts of self-care, not occasional overhauls.
Emotional balance is a key part of this. Chronic stress undermines physical health, so finding ways to manage it is essential. I incorporated practices like journaling, deep breathing, and spending time in nature. These aren’t luxuries—they’re maintenance. Social connection also plays a vital role. Strong relationships provide emotional support, reduce stress, and improve overall well-being. Making time for meaningful conversations, family dinners, or coffee with a friend isn’t frivolous—it’s protective.
Realistic pacing is another cornerstone. I learned to listen to my body’s limits and respect them. Pushing through fatigue or ignoring pain only leads to burnout. Instead, I began to honor rest as a productive act. Taking a nap, saying no to an extra commitment, or simply sitting quietly are not signs of weakness—they’re acts of wisdom. Health isn’t about doing more. It’s about sustaining what matters.
Early intervention isn’t a one-time event. It’s a lifelong practice of awareness, adjustment, and care. It’s about noticing the quiet signals—the slight dip in energy, the lingering ache, the mood shift—and responding with kindness and action. It’s about protecting your health not because you’re broken, but because you’re valuable. The body is not a machine to be driven until it fails. It’s a living system that thrives on attention, balance, and respect.
Health isn’t something we fix when it breaks—it’s what we protect every day. The real power lies not in dramatic turnarounds but in listening early, adjusting sooner, and respecting the body’s quiet signals. Small, steady choices create a life where disease doesn’t get a foothold. It’s not about being perfect. It’s about being present—before the alarm gets louder.