How I Tamed My Chronic Condition — A Real Talk on Systematic Rehab
Living with a chronic condition used to drain me—until I shifted how I approached rehab. It wasn’t about quick fixes, but building a consistent, personalized system. I started small, tracked progress, and slowly regained control. This isn’t a miracle cure, but a real, workable path. If you’re tired of feeling stuck, this journey might resonate. Always consult your doctor, but know: small steps can lead to big changes.
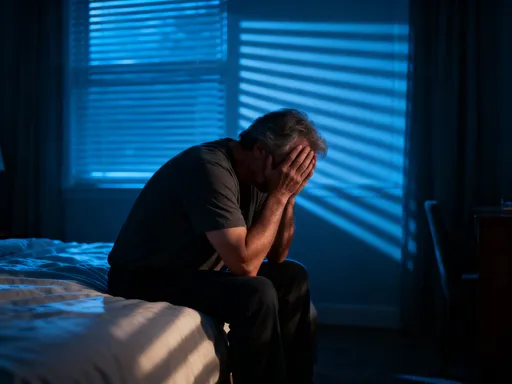
The Hidden Struggle Behind Daily Life
Chronic conditions often operate in silence, their impact felt far beyond the physical symptoms listed in medical brochures. For many women between 30 and 55, the burden is not just pain or fatigue—it’s the emotional weight of unpredictability. One day, you can manage household tasks, help the kids with homework, and even take a walk. The next, even showering feels like climbing a mountain. This inconsistency chips away at confidence, making it hard to plan, commit, or feel reliable—even to yourself.
The frustration isn’t always visible to others. Friends may say, “But you looked fine yesterday,” not realizing that “fine” is a relative term when living with a long-term health challenge. The emotional toll includes feelings of isolation, guilt, and even grief over the loss of the person you used to be—the one who could handle everything without hesitation. These emotions, if unaddressed, can deepen the cycle of fatigue and flare-ups, creating a feedback loop that standard treatments often fail to break.
Reactive care—waiting for symptoms to worsen before seeking help—is common but insufficient. It treats the fire but ignores the fuel. What many don’t realize is that chronic conditions require a shift from survival mode to management mode. This doesn’t mean resignation; it means empowerment. Instead of asking, “Why is this happening?” the more productive question becomes, “What can I do today to support my body?” That mental pivot—from helplessness to agency—is often the first real step toward meaningful progress.
Studies show that patients who adopt a proactive mindset report better quality of life, even when objective health markers remain unchanged. The reason? Control is not always about eliminating symptoms—it’s about regaining influence over your daily experience. When you stop seeing yourself as a passive recipient of treatment and start viewing yourself as an active participant in your recovery, the journey changes. This shift doesn’t happen overnight, but it can begin with a single decision: to build a system, not just endure a condition.
Why “One-Size-Fits-All” Doesn’t Work in Rehab
Standardized rehabilitation programs are designed for efficiency, not individuality. While they provide a useful starting point, they often fail to account for the unique rhythms of chronic illness. Two people with the same diagnosis may have vastly different triggers, energy patterns, and responses to treatment. One may benefit from morning movement, while another finds afternoon stretching more sustainable. One may thrive on structured routines, while another needs fluidity to adapt to daily fluctuations.
This variability is not a flaw—it’s a fact. Chronic conditions like fibromyalgia, rheumatoid arthritis, or long-term fatigue syndromes are influenced by a complex interplay of biological, environmental, and psychological factors. A treatment plan that ignores this complexity risks becoming another source of frustration. When a well-meaning therapist prescribes a fixed exercise regimen without considering your energy dips, or a nutritionist hands you a rigid meal plan that doesn’t fit your family’s schedule, the result is often discouragement, not improvement.
The key is personalization. This means learning to read your body’s signals and adjusting accordingly. It means setting goals that reflect your values, not someone else’s template. For example, if your priority is being able to play with your grandchildren without crashing afterward, your rehab should focus on stamina and recovery, not just strength or weight loss. Personalized rehab isn’t about perfection—it’s about relevance. It’s about creating a plan that fits your life, not one that forces your life to fit it.
A flexible framework allows for this. Instead of rigid rules, it offers guiding principles: listen to your body, track what works, and adjust as needed. This approach acknowledges that progress isn’t linear. Some days will be better than others, and that’s okay. The goal isn’t to follow a plan perfectly, but to stay engaged with the process. Over time, this adaptability builds resilience—the ability to respond to setbacks without losing momentum.
Building Your Rehab System: The Core Pillars
A systematic approach to rehabilitation rests on four foundational pillars: consistency, monitoring, balance, and integration. These are not flashy solutions, but quiet, reliable supports that, when combined, create lasting change. Consistency does not mean doing the same thing every day regardless of how you feel. It means showing up for your health in small, manageable ways, even when motivation is low. It’s the difference between aiming for an hour of exercise and committing to five minutes of stretching—something you can do even on tough days.
Monitoring is the practice of paying attention—not just to symptoms, but to patterns. A simple journal or a notes app can help track energy levels, sleep quality, food intake, and mood. Over time, these records reveal trends: perhaps you notice that poor sleep predicts a flare-up two days later, or that eating a balanced breakfast stabilizes your energy. This data turns guesswork into insight. It allows you to make informed choices, not just react to crises. Monitoring also reduces anxiety—when you can see progress, even if slow, it’s easier to stay the course.
Balance is about honoring both activity and rest. Many people with chronic conditions swing between overdoing it on good days and collapsing afterward, a cycle known as “push and crash.” A balanced system builds in rest proactively, not as punishment for exertion. This might mean scheduling short breaks between tasks, or planning a quiet evening after a busy morning. Balance also applies to emotional energy—setting boundaries, saying no when needed, and protecting time for activities that bring calm.
Integration means weaving rehab into daily life, not treating it as an add-on. It’s not about carving out extra time for a 30-minute workout, but finding ways to move more while folding laundry, preparing meals, or talking on the phone. It’s drinking water while watching TV, or practicing deep breathing while waiting for the kettle to boil. When rehab becomes part of your routine, it stops feeling like a chore and starts feeling like self-care. These small acts, repeated over time, build a life that supports healing—not one that fights against it.
Movement That Works—Without Overdoing It
Physical activity is often misunderstood in chronic illness. Many fear movement will make things worse, while others push too hard, hoping to “get back to normal” quickly. The truth lies in the middle: gentle, consistent movement, tailored to your capacity, is one of the most effective tools for managing symptoms. The goal is not fitness in the traditional sense, but function—being able to move through your day with less pain and more ease.
Low-impact options are ideal. Walking, even for five or ten minutes, improves circulation, supports joint health, and boosts mood. Stretching routines, done daily, maintain flexibility and reduce stiffness. Water-based exercises, such as gentle aqua aerobics, offer resistance without strain, making them excellent for those with joint pain or limited mobility. Chair yoga or seated stretches can be done at home, requiring no special equipment. The key is to start well below your limit—so low that you feel no worsening of symptoms afterward.
Gradual progression is essential. Think of it like training a muscle you didn’t know you had: your endurance for daily living. If you can walk five minutes today, aim for six next week. If you can do two sets of stretches, add a third when it feels comfortable. This slow build-up trains your body to handle more without triggering a setback. It also reinforces a sense of control—each small increase is proof that you are moving forward, even if slowly.
Listening to your body is non-negotiable. Pain is a signal, not a challenge to overcome. If an activity leaves you exhausted the next day, it was too much. Adjust accordingly. A sample weekly rhythm might include light stretching every morning, a short walk three times a week, and restorative movement like tai chi or gentle yoga on two other days. The rest of the week focuses on rest and recovery. This rhythm prevents burnout while promoting mobility, strength, and confidence in your body’s ability to heal.
Mind-Body Connection: Managing Stress & Energy
Stress is a silent amplifier of chronic symptoms. It doesn’t just affect mood—it alters physiology. When stressed, the body releases cortisol and other stress hormones, which can increase inflammation, disrupt sleep, and lower pain thresholds. For someone already managing a chronic condition, this can mean the difference between a manageable day and a flare-up. The good news is that stress is not inevitable. It can be managed, even in the midst of life’s demands.
Accessible techniques make a difference. Deep breathing, for example, activates the parasympathetic nervous system, signaling the body to relax. A simple practice—inhaling for four counts, holding for four, exhaling for six—can be done anywhere, anytime. Mindfulness, the practice of paying attention to the present moment without judgment, helps break the cycle of worry about the future or regret about the past. It doesn’t require meditation cushions or hours of silence—just a few minutes of noticing your breath, your feet on the floor, or the sounds around you.
Routine scheduling also conserves energy. Knowing what to expect reduces mental load. A predictable rhythm to your day—wake-up time, meals, rest periods—helps regulate your nervous system. It’s not about rigidity, but about creating anchors that support stability. When your day has structure, you spend less energy deciding what to do next, leaving more for the things that matter.
Emotional regulation is not a luxury—it’s a core part of rehabilitation. How you respond to frustration, disappointment, or pain influences your physical state. Responding with self-compassion—“This is hard, and I’m doing my best”—reduces internal pressure. Over time, these mental habits shape physical outcomes. You may not control your condition, but you can influence how it affects you. That shift—from reactivity to response—is where real healing begins.
Daily Habits That Add Up Over Time
Long-term improvement is not built on dramatic overhauls, but on small, repeated choices. Sleep hygiene is foundational. Going to bed and waking up at consistent times—even on weekends—helps regulate your body’s internal clock. A calming pre-sleep routine, like reading or gentle stretching, signals that it’s time to wind down. Keeping screens out of the bedroom reduces exposure to blue light, which can interfere with melatonin production.
Hydration is another simple yet powerful habit. Even mild dehydration can worsen fatigue, brain fog, and muscle cramps. Keeping a water bottle nearby and sipping throughout the day makes a difference. Nutrition basics matter, too—not extreme diets, but balanced meals with protein, fiber, and healthy fats to stabilize energy. Eating regularly prevents blood sugar crashes that can mimic or worsen symptoms.
Pacing activities is perhaps the most transformative habit. Breaking tasks into smaller chunks—folding half the laundry now, the rest later—prevents overexertion. Setting rest reminders on your phone ensures you take breaks before you feel exhausted. Using a timer to work in 20-minute intervals, followed by 10 minutes of rest, creates a sustainable rhythm. These strategies are not signs of weakness—they are tools of wisdom.
Over time, these habits compound. You may not notice change day to day, but after weeks or months, you’ll realize you’re doing more with less effort. You’re sleeping better, thinking more clearly, and moving with greater ease. The power lies in consistency, not intensity. You don’t have to be perfect—just persistent. Each small choice is a vote for the kind of life you want to live.
Staying on Track: Adjusting, Not Quitting
Setbacks are not failures—they are part of the process. Plateaus happen. Flare-ups occur. Some weeks, progress feels invisible. The key is to respond with compassion, not criticism. When you miss a day of stretching or push too hard on a walk, the goal is not to punish yourself, but to learn. Ask: What led to this? Was I too optimistic? Did stress pile up? Was I ignoring early warning signs?
Regular review is essential. Every few weeks, take time to reflect. What’s working? What isn’t? Are your goals still meaningful? Adjust your system as needed. Maybe you need to reduce activity after a busy week, or add more rest days. Perhaps tracking symptoms reveals a pattern you hadn’t noticed—like caffeine affecting your sleep. These insights allow you to refine your approach, making it more effective and sustainable.
Motivation will ebb and flow. That’s normal. What matters is commitment to the process, not the feeling of enthusiasm. On low-motivation days, rely on your system: do the minimum version of your routine, just to stay connected. Trust that showing up, even in a small way, keeps the momentum alive. Celebrate effort, not just outcomes. Finishing a gentle stretch session on a tough day is a win.
Always work with healthcare providers. Share your tracking data, ask for feedback, and collaborate on adjustments. This isn’t about replacing medical advice—it’s about enhancing it with your lived experience. Your doctor knows medicine; you know your body. Together, you can create a rehab plan that is both scientifically sound and personally meaningful.
Conclusion: A Life Reclaimed, Step by Step
Reclaiming your life with a chronic condition isn’t about dramatic transformations—it’s about steady, intentional steps. A systematic, patient-centered approach turns overwhelming challenges into manageable actions. It replaces helplessness with agency, confusion with clarity, and isolation with empowerment. This journey isn’t linear, and it doesn’t promise perfection. But it does offer progress—measured not in miles walked or pounds lost, but in moments of ease, confidence, and connection.
The power lies in consistency, not intensity. In showing up for yourself, day after day, with kindness and patience. In building a system that honors your limits while gently expanding them. In trusting that small choices, repeated over time, create lasting change. You don’t have to do everything at once. You just have to start—where you are, with what you have. And remember: you are not alone. Millions are walking this path, learning, adjusting, and moving forward. With the right support and the right mindset, you can too. Always consult your healthcare provider, but also trust your own experience. Your journey is yours—and it matters.