What Changed My Recovery? A Real Talk on Women’s Healing
Recovering from physical or emotional setbacks isn’t just about time—it’s about how you move, rest, and care for yourself. As women, our bodies go through unique changes and challenges that need thoughtful attention. I’ve been there—feeling stuck, tired, unsure where to start. This plan isn’t magic, but it’s made a real difference. Let me share what actually worked when I took my healing into my own hands. It wasn’t about pushing harder or following trends. It was about listening—really listening—to what my body was trying to say. And in doing so, I found a way forward that felt sustainable, gentle, and deeply personal.
Understanding Women’s Unique Recovery Needs
Women’s bodies are not simply smaller versions of men’s—they operate on different physiological rhythms that significantly affect how recovery unfolds. Hormonal fluctuations across the menstrual cycle, for example, influence inflammation levels, muscle repair speed, and pain sensitivity. Estrogen and progesterone play active roles in tissue healing and immune response, meaning a woman’s recovery capacity can vary week to week. During the luteal phase, when progesterone rises, some women experience increased joint laxity and fatigue, making them more prone to injury or slower healing. Meanwhile, metabolic rates in women tend to be more responsive to stress and caloric intake, which can impact energy availability for recovery processes.
Common challenges women face after illness or injury go beyond physical symptoms. Many report persistent fatigue that doesn’t improve with sleep, joint discomfort even with minor activity, and emotional volatility such as mood swings or low motivation. These are not signs of weakness—they are signals that the body is working hard to restore balance. Yet, standard rehabilitation programs often overlook these nuances. Most clinical guidelines and fitness-based recovery plans are based on male-dominant research, which means women may be pushed into routines that don’t align with their biological needs. For instance, expecting the same strength training progression for a postpartum woman as for a male athlete ignores the profound changes in connective tissue and core integrity after childbirth.
The consequence of this one-size-fits-all approach is often frustration and setbacks. Women may feel discouraged when they don’t respond to treatment the way others do, leading to self-blame or premature discontinuation of care. Recognizing that recovery is not linear—and that female physiology requires tailored support—is the first step toward meaningful healing. This doesn’t mean creating entirely separate systems, but rather adapting existing frameworks to honor hormonal cycles, metabolic sensitivity, and emotional resilience. When care plans consider these factors, women are more likely to experience consistent progress without burnout or re-injury.
The Mindset Shift That Starts Healing
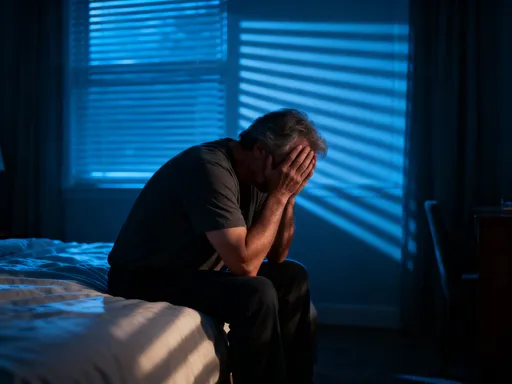
One of the most transformative moments in my recovery was realizing that healing is not a race. For years, I measured progress by speed—how quickly I could return to work, resume exercise, or fit into old clothes. But this mindset set me up for repeated setbacks. The turning point came when I began to redefine what progress meant. Instead of asking, “Am I better yet?” I started asking, “Did I honor my body today?” This subtle shift—from performance to presence—changed everything. Healing isn’t about bouncing back; it’s about building forward with greater awareness and care.
Self-compassion became the foundation of this new mindset. Too often, women are conditioned to push through discomfort, to be strong for others, to minimize their own needs. But in recovery, this pattern can be harmful. Ignoring pain or fatigue doesn’t make you resilient—it delays healing. The idea that rest is a sign of weakness is a myth that needs to be dismantled. In reality, rest is an active part of recovery. It’s during rest that cells repair, hormones rebalance, and the nervous system recalibrates. When you allow yourself to pause, you’re not giving up—you’re giving your body the space it needs to rebuild.
Patience, too, is not passive. It’s a practice of trust—trusting that your body knows how to heal, even if the timeline isn’t predictable. This doesn’t mean ignoring medical advice or avoiding action. It means balancing effort with acceptance. Some days will feel like steps forward; others may feel like setbacks. But each day offers an opportunity to learn—about your limits, your triggers, and your strengths. By replacing self-criticism with curiosity, you create an internal environment where healing can thrive. This mindset isn’t just helpful—it’s necessary for sustainable recovery.
Building a Daily Rhythm That Supports Recovery
Consistency is one of the most underrated tools in recovery. While dramatic changes often get attention, it’s the small, repeated actions that create lasting results. Establishing a daily rhythm—a predictable structure for sleep, movement, nourishment, and rest—can significantly enhance the body’s ability to heal. The human body thrives on routine, especially during periods of recovery when energy is limited and systems are sensitive. A steady rhythm reduces decision fatigue, supports hormonal balance, and creates a sense of safety that allows the nervous system to shift from survival mode to repair mode.
Sleep is the cornerstone of this rhythm. Quality rest is when tissue repair occurs, inflammation is regulated, and emotional processing takes place. For women, disrupted sleep can worsen hormonal imbalances and prolong recovery. Aim for consistent bedtime and wake-up times, even on weekends. Create a wind-down routine—dimming lights, reducing screen time, and engaging in calming activities like reading or gentle stretching. The goal isn’t perfection, but regularity. Even modest improvements in sleep quality can lead to noticeable changes in energy, mood, and pain levels.
Morning habits also set the tone for the day. Instead of rushing into tasks, begin with a few minutes of stillness—deep breathing, hydration, or a brief check-in with how your body feels. This practice fosters body awareness and helps you make choices that support recovery rather than deplete energy. Throughout the day, practice pacing—alternating periods of activity with intentional rest. This might mean sitting down after standing for 20 minutes, or taking a five-minute breathing break between tasks. These pauses are not luxuries; they are essential for preventing flare-ups and maintaining steady progress.
A sample day might include waking at the same time daily, drinking water upon rising, engaging in 10 minutes of gentle movement, eating a nourishing breakfast, and scheduling tasks with built-in rest periods. Include mental breaks—short walks, quiet moments, or listening to calming music. The structure doesn’t need to be rigid, but having a general flow helps reduce stress and supports the body’s natural healing cycles. Over time, this rhythm becomes a form of self-respect—a daily commitment to your well-being.
Movement That Helps, Not Hurts
Movement is essential for recovery, but not all movement is beneficial at every stage. For many women, the instinct after injury or illness is either to stop moving entirely or to jump back in too quickly. Both extremes can hinder healing. The key is finding the right type and amount of activity—one that supports circulation, maintains mobility, and builds strength without causing strain. Low-impact exercises are often the most effective during recovery. Walking, for example, improves blood flow, reduces inflammation, and supports mental well-being without placing excessive stress on joints or tissues.
Pelvic floor activation and gentle core engagement are also important, especially for women who have experienced pregnancy, surgery, or chronic stress. These muscles play a critical role in stability, posture, and organ support. Simple exercises like diaphragmatic breathing with pelvic floor lifts can be done lying down and require minimal effort, yet they lay the foundation for stronger, more resilient movement over time. Light resistance training with bands or small weights can help rebuild muscle mass without overloading the system, as long as intensity is carefully monitored.
The danger of high-intensity workouts too soon lies in their potential to trigger inflammation, delay tissue repair, and increase injury risk. When the body is in recovery mode, its capacity to handle stress is reduced. Pushing through fatigue or pain may feel productive in the moment, but it often leads to setbacks. Instead, the focus should be on listening—paying attention to signals like increased heart rate, joint discomfort, or prolonged soreness. These are not signs to push harder, but cues to adjust. Movement should leave you feeling energized, not drained.
Integrating movement into daily life doesn’t require a gym or strict schedule. It can be as simple as stretching while waiting for coffee, taking the stairs slowly, or doing seated leg lifts during a phone call. The goal is consistency, not intensity. Over time, these small efforts build resilience and confidence. Movement becomes less about performance and more about partnership—with your body, your pace, and your healing journey.
Nutrition as Nourishment, Not Perfection
Nutrition plays a vital role in recovery, but it doesn’t require strict diets or obsessive tracking. The goal is not to achieve an ideal weight or follow the latest trend, but to provide the body with the building blocks it needs to repair tissues, balance hormones, and sustain energy. Whole, minimally processed foods are the foundation of this approach. Vegetables, fruits, lean proteins, healthy fats, and whole grains offer a spectrum of nutrients that support cellular regeneration and immune function. The focus should be on inclusion—adding nourishing foods—rather than restriction.
Specific nutrients are particularly important for women in recovery. Iron, for example, supports oxygen transport and energy production, and deficiencies are common, especially among those with heavy menstrual cycles. Magnesium plays a role in muscle relaxation, nerve function, and sleep regulation—making it essential for recovery from both physical and emotional stress. Protein is critical for tissue repair, and adequate intake helps prevent muscle loss during periods of reduced activity. These nutrients can be obtained through food: spinach and lentils for iron, nuts and seeds for magnesium, and eggs, fish, or legumes for protein.
Eating intuitively—paying attention to hunger, fullness, and satisfaction—can help align food choices with healing needs. This doesn’t mean ignoring structure, but rather tuning in to what the body truly needs each day. Some days may call for more carbohydrates to support energy; others may require extra protein for repair. The goal is flexibility, not rigidity. Avoiding extreme diets or calorie restriction is crucial, as these can disrupt hormonal balance and slow recovery. Instead, aim for regular meals and snacks that combine protein, fiber, and healthy fats to maintain steady energy and support satiety.
Nutrition is not about perfection. It’s about consistency and care. A nourishing meal doesn’t have to be gourmet—it can be a bowl of oatmeal with fruit and nuts, a simple soup with vegetables and beans, or a grilled fish with roasted sweet potatoes. What matters is that it supports your body’s needs without adding stress. When food is viewed as fuel for healing rather than a source of guilt or control, it becomes a powerful ally in recovery.
Emotional Support and Social Connection
Healing is not just a physical process—it’s deeply emotional. Yet, many women try to go through recovery in silence, fearing they’ll be seen as weak or burdensome. This isolation can slow progress. Research consistently shows that social support improves recovery outcomes, reducing stress, enhancing mood, and even speeding tissue repair. Talking about your experience—whether with a trusted friend, a support group, or a therapist—creates space for emotional release and validation. It reminds you that you’re not alone, and that your feelings are part of the process, not a sign of failure.
Finding safe spaces to share is essential. This might be an in-person support group for women recovering from similar conditions, an online community, or regular check-ins with a close friend. The key is consistency and trust. These connections don’t have to be deep or lengthy—sometimes a brief conversation can lift a heavy emotional load. What matters is that you feel heard and understood. Sharing your story can also help others, creating a ripple effect of support and encouragement.
At the same time, protecting your emotional energy is just as important as physical rest. Not every conversation is helpful. Some people may offer unsolicited advice, minimize your experience, or drain your energy with their own stress. Learning to set boundaries—saying no to draining interactions, limiting time with negative influences, or postponing difficult conversations—is a form of self-care. It’s not selfish; it’s necessary for healing. You don’t have to explain or justify your needs. Protecting your peace is a legitimate and vital part of recovery.
Emotional support isn’t a luxury—it’s a biological necessity. Chronic stress increases cortisol, which can impair immune function and delay healing. Positive social interactions, on the other hand, trigger the release of oxytocin and other calming hormones that support repair. When you feel seen and supported, your body can shift out of survival mode and into healing mode. This is why connection isn’t just comforting—it’s therapeutic.
Tracking Progress Without Obsession
Measuring progress is important, but the way you track can either support or sabotage recovery. Many women fall into the trap of obsessing over numbers—weight, steps, calories, or workout intensity. While data can be useful, it often becomes a source of stress when it replaces bodily awareness. A more sustainable approach is gentle tracking—using simple tools like a journal or mood log to notice subtle changes over time. These might include sleeping through the night, feeling less joint stiffness in the morning, or completing a task without exhaustion. These small victories are real progress, even if they don’t show up on a scale.
Non-scale victories are often the most meaningful. Improved sleep quality, increased mental clarity, reduced pain, or the ability to engage in a favorite activity are all signs of healing. Celebrating these moments reinforces positive behavior and builds motivation. Instead of asking, “How far do I have to go?” try asking, “How far have I come?” This shift in perspective fosters gratitude and resilience. It reminds you that healing is happening, even when it’s slow or invisible.
Tracking should be informative, not punitive. If reviewing your notes makes you feel discouraged, it’s time to adjust your method. Keep it simple: one sentence per day about how you felt, what you did, and what supported you. Over weeks, patterns will emerge—what helps, what doesn’t, and how your body responds to different choices. This knowledge empowers you to make informed decisions without relying solely on external guidance.
Finally, tracking also helps identify when to seek professional support. If fatigue persists despite rest, pain worsens, or emotional distress increases, it’s a signal to consult a healthcare provider. This plan is designed to complement medical care, not replace it. There is no shame in needing help. In fact, recognizing when to reach out is one of the strongest things you can do for your recovery.
Conclusion
True rehabilitation isn’t about rushing back to “normal”—it’s about rebuilding with intention. For women, honoring biological rhythms and emotional needs makes all the difference. This approach isn’t a shortcut, but a sustainable way to heal deeper and stronger. When you listen closely, your body tells you exactly what it needs. Recovery is not a test of endurance, but an invitation to reconnect—with your body, your pace, and your inner wisdom. By embracing rest, nourishment, gentle movement, and connection, you create the conditions for lasting healing. It won’t always be linear, but each step forward, no matter how small, is a victory. And in that quiet, consistent care, real transformation begins.