Why Better Sleep Changed My Health Game Forever
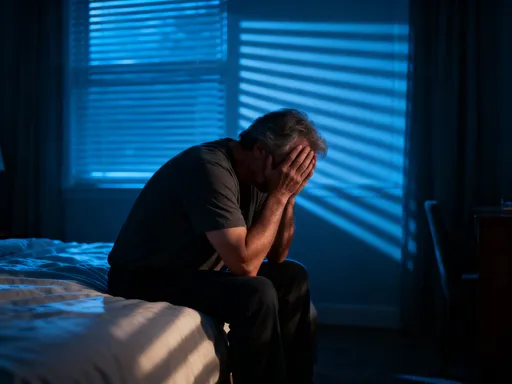
Sleep used to be the last thing I prioritized—until chronic fatigue and mood swings started affecting my daily life. I realized poor sleep wasn’t just about tiredness; it was making my health struggles worse. After working with doctors and testing small but powerful changes, I saw real improvements. This is how upgrading my sleep quality became a key part of managing my long-term health—naturally, safely, and effectively.
The Hidden Cost of Poor Sleep in Chronic Health Conditions
For many women in their 30s, 40s, and 50s, managing a chronic health condition is already a full-time job. Between doctor visits, medication schedules, and daily symptom tracking, sleep often falls to the bottom of the priority list. Yet, consistently poor sleep can quietly undermine even the most carefully managed health plans. It’s not just about feeling groggy in the morning—lack of quality rest affects the body’s ability to regulate key systems that influence long-term well-being.
One of the most significant impacts of disrupted sleep is on the immune system. During deep sleep, the body produces cytokines—proteins that help fight infection and inflammation. When sleep is cut short or fragmented, this production slows, leaving the body more vulnerable to flare-ups and slower healing. For someone managing conditions like rheumatoid arthritis or lupus, this can mean longer recovery times and increased discomfort. Poor sleep has also been linked to elevated levels of C-reactive protein, a marker of systemic inflammation, which is a common thread in many chronic illnesses.
Hormone regulation is another critical area affected by sleep quality. The body’s stress hormone, cortisol, follows a natural rhythm that depends on consistent sleep patterns. When sleep is erratic, cortisol levels can remain elevated, contributing to insulin resistance, weight gain, and blood pressure fluctuations. For women managing type 2 diabetes or hypertension, this disruption can make it harder to maintain stable readings, even with medication. The connection is clear: poor sleep doesn’t just accompany health challenges—it can actively worsen them.
Consider a real-life scenario: a woman in her late 40s with Hashimoto’s thyroiditis pushes through a busy week, sacrificing sleep to keep up with family and work demands. She notices increased fatigue and joint pain but attributes it to stress. Without adequate rest, her immune system remains overactive, and her thyroid antibodies rise. Her doctor adjusts her medication, but the root cause—chronic sleep deprivation—goes unaddressed. This pattern repeats, leading to a cycle of worsening symptoms and frustration. It’s a common story, yet one that can be broken with greater awareness.
The truth is, sleep is not a luxury. It is a biological necessity, as essential as nutrition and physical activity. For women managing long-term health conditions, treating sleep as a core component of care—not an afterthought—can lead to meaningful improvements in daily function and disease stability. Recognizing this shift in mindset is the first step toward lasting change.
What Science Says: The Link Between Sleep Quality and Disease Control
Over the past two decades, scientific research has increasingly confirmed what many women intuitively feel: high-quality sleep plays a vital role in managing chronic illness. It’s not just about the number of hours spent in bed, but the depth and continuity of sleep that determine its healing power. During restorative sleep, particularly in the deep stages of non-REM and REM cycles, the body engages in essential repair processes—from cellular regeneration to memory consolidation.
One of the most compelling findings is how sleep supports metabolic health. Studies show that even one night of poor sleep can impair glucose metabolism, mimicking early signs of insulin resistance. For individuals with prediabetes or type 2 diabetes, this means that inconsistent sleep can lead to higher blood sugar levels the following day, regardless of diet or medication. Over time, this contributes to greater difficulty in disease control and increases the risk of complications. The body’s ability to regulate insulin is closely tied to circadian rhythm, the internal 24-hour clock that governs hormone release, digestion, and body temperature.
The circadian rhythm is highly sensitive to environmental cues, especially light and darkness. When sleep schedules are irregular—going to bed late one night, waking early the next—the body’s internal clock becomes misaligned. This misalignment, known as circadian disruption, has been linked to increased inflammation, hormonal imbalances, and impaired immune response. Think of it like a factory assembly line: if the timing is off, even high-quality parts won’t come together properly. In the same way, when the body’s systems are out of sync due to poor sleep, healing and regulation suffer.
Deep sleep, also called slow-wave sleep, is particularly important for physical recovery. During this phase, the body releases growth hormone, repairs tissues, and clears out metabolic waste from the brain. For someone recovering from a flare-up of an autoimmune condition or managing chronic pain, this nightly maintenance is crucial. Without sufficient deep sleep, the body remains in a state of partial stress, unable to fully reset. Fragmented sleep—waking up multiple times or spending too much time in light sleep—prevents the brain and body from entering these restorative phases consistently.
Another key insight from sleep research is the connection between sleep and emotional regulation. The prefrontal cortex, responsible for decision-making and emotional control, is highly dependent on rest. When sleep is inadequate, this brain region becomes less effective, leading to increased irritability, brain fog, and reduced resilience to stress. For women juggling family, work, and health concerns, this can create a feedback loop: poor sleep leads to stress, which further disrupts sleep. Breaking this cycle requires recognizing sleep not as a passive state, but as an active investment in mental and physical stability.
The evidence is clear: sleep is not downtime. It is a dynamic, biologically active process that directly influences disease outcomes. By prioritizing consistent, high-quality rest, women can support their body’s natural ability to heal, regulate, and adapt—making it a powerful, non-pharmacological tool in long-term health management.
Spotting the Signs: Is Your Sleep Sabotaging Your Health?
Many women assume that if they can fall asleep and stay in bed for seven or eight hours, their sleep must be fine. But quantity doesn’t always equal quality. The real question is: do you wake up feeling refreshed? If the answer is often no, it’s possible that your sleep is working against your health goals, even if you’re not fully aware of it. Recognizing the subtle signs of poor sleep is the first step toward making meaningful changes.
One common red flag is frequent nighttime awakenings. Waking up two or more times per night, especially if it takes effort to fall back asleep, disrupts the sleep cycle and prevents the body from reaching deep, restorative stages. This kind of fragmented sleep can leave you feeling tired despite spending enough time in bed. Another sign is non-refreshing sleep—when you wake up after a full night’s rest but still feel heavy, drained, or mentally foggy. This is often linked to poor sleep quality rather than lack of sleep duration.
Daytime symptoms are also important clues. Persistent brain fog, difficulty concentrating, or needing multiple cups of coffee to stay alert may indicate that your brain didn’t get the rest it needed. Mood changes, such as increased irritability or low motivation, can also stem from poor sleep. These symptoms are often dismissed as part of aging or stress, but they may actually be signals that your body is not recovering properly at night.
For women managing chronic conditions, these sleep-related symptoms can have a direct impact on disease control. For example, someone with fibromyalgia may notice that their pain levels increase after a night of poor sleep. A woman with hypertension might find her blood pressure harder to manage on days following disrupted rest. These patterns are not coincidental—they reflect the body’s heightened sensitivity to sleep deprivation when it’s already under stress from illness.
Another overlooked sign is reliance on naps. While short, early-afternoon naps can be beneficial, frequent or long daytime sleeping may indicate that nighttime rest is insufficient. If you find yourself needing to nap regularly just to function, it’s worth examining your sleep habits more closely. Similarly, relying on sleep aids—whether over-the-counter supplements or prescription medications—can mask underlying issues without addressing the root cause.
The good news is that awareness can lead to change. Keeping a simple sleep journal for a week—tracking bedtime, wake time, nighttime awakenings, and how you feel in the morning—can reveal patterns that might otherwise go unnoticed. This kind of self-monitoring doesn’t require special tools or expertise; it’s a practical way to gather personal data and start a more informed conversation with your healthcare provider. By paying attention to these signs, you take an active role in protecting your long-term health.
Building a Real-World Sleep Routine That Works
Knowing that sleep matters is one thing; actually improving it is another. The key to lasting change is not drastic overhauls, but small, consistent habits that fit into real life. A sustainable sleep routine doesn’t require perfection—it requires intention. The goal is to create conditions that signal to your body and brain that it’s time to wind down, making it easier to fall asleep and stay asleep through the night.
One of the most effective steps is setting a consistent bedtime and wake time, even on weekends. The body thrives on routine, and a stable sleep schedule helps reinforce the circadian rhythm. While it may not always be possible to go to bed at the exact same time every night, aiming for a window of no more than an hour’s variation can make a noticeable difference. Waking up at roughly the same time each morning, regardless of when you fell asleep, helps anchor your internal clock and improves sleep quality over time.
Equally important is the wind-down routine. Just as children benefit from a bedtime ritual, adults do too. This doesn’t have to be elaborate—15 to 30 minutes of calming activity can be enough. Reading a physical book, practicing gentle stretching, or listening to soft music are all effective ways to transition from the busyness of the day to a state of relaxation. The key is to choose activities that are low-stimulation and screen-free, as blue light from phones, tablets, and TVs can suppress melatonin, the hormone that regulates sleep.
Your sleep environment also plays a crucial role. A cool, dark, and quiet bedroom supports deeper sleep. Most experts recommend a room temperature between 60 and 67 degrees Fahrenheit (15–19°C) for optimal rest. Blackout curtains, a comfortable mattress and pillows, and minimizing noise—either through soundproofing or a white noise machine—can all contribute to a more restful space. If outside noise is unavoidable, a fan or a sound machine with nature sounds can help mask disruptions.
Personal experience shows that small adjustments can have big impacts. One woman in her 50s found that switching from late-night television to reading a novel helped her fall asleep 20 minutes faster and reduced nighttime awakenings. Another started doing five minutes of deep breathing before bed and noticed improved morning alertness within a week. These changes didn’t require extra time or expense—they simply involved making sleep a conscious priority.
Consistency is more important than perfection. Missing a night or two of good sleep doesn’t undo progress. What matters is returning to the routine without guilt or frustration. Over time, these small efforts build momentum, leading to more stable sleep patterns and better overall health.
Lifestyle Tweaks That Boost Sleep Naturally
Sleep doesn’t happen in isolation. What you do during the day has a direct impact on how well you sleep at night. Many women focus on bedtime habits but overlook the daytime behaviors that set the stage for rest. By making a few strategic adjustments to your daily routine, you can naturally enhance your body’s ability to fall and stay asleep.
Exposure to natural light is one of the most powerful tools for regulating sleep. Sunlight, especially in the morning, helps reset the circadian rhythm and promotes alertness during the day. Spending even 15 to 30 minutes outside in the morning—whether walking the dog, having coffee on the porch, or gardening—can improve nighttime sleep quality. If outdoor time is limited, sitting near a bright window can also help. The key is getting light exposure early in the day, not late in the afternoon or evening, which can interfere with melatonin release.
Physical activity is another important factor. Regular exercise has been shown to reduce the time it takes to fall asleep and increase deep sleep duration. However, the timing of workouts matters. Exercising too close to bedtime—within two to three hours—can raise body temperature and stimulate the nervous system, making it harder to wind down. Shifting workouts to the morning or early afternoon can maximize sleep benefits while minimizing nighttime disruption.
Diet also plays a role. Large, heavy meals late in the evening can cause discomfort and indigestion, interfering with sleep. Eating dinner at least two to three hours before bed allows time for digestion. Additionally, certain substances can subtly affect sleep architecture. Caffeine, even in moderate amounts, can stay in the system for six to eight hours. A late afternoon coffee or tea might not keep you awake, but it can reduce deep sleep and increase nighttime awakenings. Switching to herbal tea or decaffeinated options after 2 p.m. can make a noticeable difference.
Alcohol is another common sleep disruptor. While it may help some people fall asleep faster, it often leads to fragmented sleep later in the night, reducing REM sleep and overall sleep quality. For women managing chronic conditions, this disruption can be especially problematic. Reducing alcohol intake, particularly in the evening, supports more restorative rest. Instead, consider calming alternatives like chamomile tea, warm milk, or a small snack with tryptophan-rich foods like bananas or nuts.
Hydration is important, but timing matters. Drinking large amounts of fluids right before bed can lead to frequent nighttime bathroom trips. Spreading fluid intake throughout the day and reducing it in the evening can help minimize disruptions. At the same time, mild dehydration can cause muscle cramps or discomfort, so it’s important to find a balance.
These lifestyle tweaks don’t require drastic changes. They’re about making small, intentional choices that support your body’s natural rhythms. Over time, they create a foundation for better sleep—one that works with your biology, not against it.
When to Seek Help: Working With Professionals
While many sleep issues can be improved with lifestyle changes, some require professional evaluation. It’s important to recognize when poor sleep may be a sign of an underlying condition that needs medical attention. Sleep apnea, for example, is a common but often undiagnosed disorder, particularly in middle-aged women. Symptoms include loud snoring, gasping for air during sleep, and excessive daytime fatigue despite adequate sleep duration. Left untreated, sleep apnea can worsen hypertension, increase cardiovascular risk, and interfere with chronic disease management.
Chronic insomnia is another condition that may benefit from clinical support. If you’ve been struggling with difficulty falling or staying asleep for more than three months, despite consistent efforts to improve sleep habits, it may be time to consult a healthcare provider. Cognitive behavioral therapy for insomnia (CBT-I) is a highly effective, non-drug treatment that addresses the thoughts and behaviors that contribute to sleep difficulties. Unlike sleep medications, which can have side effects and lead to dependency, CBT-I offers long-term solutions.
Other signs that warrant professional input include restless legs syndrome, frequent nighttime urination, or unexplained drops in energy that coincide with poor sleep. These symptoms may point to hormonal imbalances, neurological issues, or medication side effects. A doctor can help determine whether further testing—such as a sleep study—is needed.
It’s also important to discuss sleep concerns during regular health check-ups, especially if you’re managing a chronic condition. Many women hesitate to bring up sleep issues, fearing they’ll be dismissed as normal aging or stress. But sleep is a vital sign of overall health, and healthcare providers are increasingly recognizing its importance. Open, honest conversations can lead to personalized recommendations, whether it’s adjusting medication timing, addressing anxiety, or referring to a sleep specialist.
Working with professionals doesn’t mean giving up control—it means gaining support. A collaborative approach ensures that sleep improvements are safe, effective, and aligned with your overall health plan. Whether through therapy, medical treatment, or simple adjustments, professional guidance can help you achieve better rest without guesswork.
Sleep as a Daily Act of Self-Care—Not a Side Task
At its core, sleep is an act of self-care. It is a daily commitment to your body’s need for repair, regulation, and renewal. For women who often put everyone else’s needs first, prioritizing sleep can feel indulgent or even selfish. But the truth is, taking care of yourself enables you to care for others more effectively. When you sleep well, you have more energy, better focus, and greater emotional resilience—qualities that benefit your entire household.
Better sleep doesn’t have to be complicated. It starts with a shift in mindset: viewing rest not as wasted time, but as essential maintenance. Just as you wouldn’t skip a medication or ignore a doctor’s advice, you can choose to treat sleep with the same level of respect. Small, consistent actions—going to bed at a regular time, creating a calming routine, adjusting daily habits—add up to meaningful change.
The benefits extend far beyond feeling more alert. Over time, improved sleep can lead to better disease management, reduced inflammation, and enhanced mood. It supports heart health, cognitive function, and emotional balance. Most importantly, it gives you a greater sense of control over your well-being. You’re not just surviving each day—you’re thriving.
Every woman’s journey is different, but the goal is the same: to feel stronger, healthier, and more in tune with your body. Better sleep is not a miracle cure, but it is a powerful ally. It is achievable, within reach, and worth the effort. By making sleep a non-negotiable part of your daily routine, you invest in a future of greater health, vitality, and peace of mind.